Introduction
Psychosis is a symptom that is displayed in several different types of mental health disorders (such as Schizophrenia). It involves impairment in functioning and distorted reality, in the form of hallucinations and/or delusions. Not everyone who has psychosis will experience it in the same way.
Hallucinations and Delusions
Hallucinations involve the experience of sensory perceptions without an actual stimulus. For instance, this can include hearing or seeing something that is not actually there. Hallucinations are divided into sensory hallucinations (i.e., feeling things on your body); visual hallucinations (i.e., seeing objects or figures that are not actually there); and auditory hallucinations (i.e., hearing sounds or voices that others cannot hear).
Delusions are thoughts or beliefs that are contrary to the evidence. For instance, this may include a belief that the television is talking to you. There are different types of delusions, such as delusions of paranoia, somatic delusions, and grandiose delusions. Paranoid delusions may include beliefs that the government is following you; somatic delusions can include beliefs that you are ill when you are actually healthy; and grandiose delusions can include beliefs that overestimate your power or importance.
Other Symptoms of Psychosis
Other signs and symptoms of psychosis may include:
- Withdrawal from others
- Loss of motivation
- Feelings of anxiety or depression
- Changes in sleep
- Cognitive problems (e.g., difficulties concentrating, remembering, reasoning, processing information, problem solving, planning ahead)
- Thoughts may seem blocked, sped up, or slowed
- Substance use
- Self-harm
- Bizarre or unusual behaviour
- Suspiciousness
- Decreased reactions to the environment
- Difficulty carrying out daily tasks/activities
- Disorganized speech
- Catatonia
Disorganized Speech
Disorganized speech is one of the symptoms of psychosis. It can present in different manners, such as quickly changing topics in conversation, “word salad” (putting words together that do not make sense in a sentence), using made-up words, repeating words or sentences, or echoing what a person is saying. It can also include very rapid speech that may interfere with one’s ability to communicate properly.
Catatonia
Catatonia is sometimes demonstrated in individuals with psychosis. It typically includes the presence of three or more motor or speech abnormalities, such as lack of spontaneous activity, mutism, repetitive behaviour, grimacing, or echoing another person’s speech/movements.
Categorization of Symptoms
Symptoms of psychosis as well as some disorders characterized by psychosis (such as Schizophrenia) are divided into two categories: positive and negative symptoms. Positive symptoms are “added” to a person’s experiences and perceptions (e.g., paranoia or hearing voices), while negative symptoms include behaviours or thoughts that are “taken away” or reduced (e.g., reduced motivation or reduced intensity of emotion).
Men who are at risk of developing psychosis have more severe negative symptoms than women before the onset of a psychotic episode. This sometimes makes it more challenging to detect, as current mental health assessments usually focus on positive symptoms (Barajas et al., 2015).
Symptom Development
Sometimes, there is an absence of symptoms prior to a psychotic episode, or symptoms of minimal severity. This occurs during the first of three common stages of psychosis (prodrome stage), and it is sometimes challenging to identify early. For instance, the individual may feel “different” or “not like themselves” but be unable to identify any specific issues. Over time, additional symptoms may develop, leading to impairment in self-care, relationships, hobbies, and school/work. This is the second stage (acute stage). The last stage (recovery) focuses on treatment and remission.
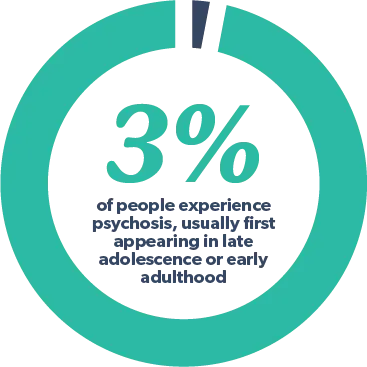
Approximately three per cent of people will have an episode of psychosis at some stage in their life, although symptoms typically have their initial onset in late adolescence or early adulthood (Fraser Health, 2018).
When the individual experiences psychotic symptoms, it usually develops over a period of hours or days. During this time, they may behave in unpredictable or unusual ways. Usually psychosis is known for the individual having a lack of insight, but this is not always the case. Insight refers to an individual’s awareness about their health condition and how it is affecting them. For instance, someone who is psychotic may not be aware that they have a problem or do not believe that their behaviours are problematic. However, loved ones or other individuals close to the individual are usually able to identify that there is a mental health problem. As such, a lack of insight in the individual may prevent them from seeking help in a timely manner; it may also make it challenging for loved ones to seek assistance for the individual on their behalf. In addition, there are many negative myths about psychosis and psychotic disorders in the media/society that may also serve as a barrier to receiving timely intervention.
Myths Pertaining to Psychosis
Several common myths and misconceptions associated with psychosis are discussed below.
Myth: People with psychosis are psychopaths.
Fact: There is a difference between having psychosis or a psychotic disorder and psychopathy.
Psychosis involves distorted reality perception (commonly in the form of hallucinations and delusions). In contrast, psychopathy describes a mental health issue characterized by manipulation or abuse of others to obtain personal goals/desires. Often others are harmed physically and/or emotionally in the process. However, individuals with psychosis will typically not cause deliberate harm to others.
Myth: People experiencing psychosis are dangerous and should be avoided.
Fact: Individuals with psychosis are not likely to deliberately harm others.
Individuals with psychosis experience a break from reality. When this occurs, they may be anxious, emotionally dysregulated, and/or unable to perceive potential hazards (e.g., not able to recognize traffic signals and attempt to cross a road with oncoming traffic). However, in a general sense, individuals with psychosis are not typically violent or overly aggressive. They usually do not cause deliberate harm to others.
Myth: Psychosis is caused by bad parenting.
Fact: Psychosis is not caused by any one particular thing.
Some people believe that an individual with psychosis or a psychotic disorder was neglected or raised incorrectly, which caused them to eventually develop a psychotic condition. It is important to note that psychosis is not merely a behavioural problem or something that can be easily controlled.
Neglectful parenting and excessive stress in early childhood may place an individual at increased risk of developing psychosis, but there are usually other factors that interact with one’s genetics to increase one’s risk of developing it. For instance, stress in adulthood, abuse/trauma, lack of sleep, and alcohol/drug use are factors. Indeed, you are more likely to develop psychosis or a psychotic disorder if you have a close family member with Schizophrenia or Bipolar Disorder. Research has also found that a genetic mutation known as 22q11.2 deletion syndrome may increase one’s risk for developing a psychotic disorder as well. Changes in hormones after pregnancy and changes in brain structure may also contribute to its development.
There are also certain illnesses that can cause psychosis, such as Parkinson’s disease, Huntington’s disease, some chromosomal disorders, brain tumors, certain types of dementia (e.g., Alzheimer’s disease), HIV, epilepsy, and stroke.
Myth: People with psychosis are all the same.
Fact: There are many different types of psychosis and psychotic disorders.
Psychosis may present very differently depending on the individual. This can be dependent on the age, gender, and ethnicity of the individual, along with their genetics, environment, and prior experiences/mental health issues. Here are some of the most common types of psychosis:
This occurs during times of extreme stress or trauma (e.g., sudden loss of a loved one). Psychotic symptoms typically last for a few days, up to a month, depending on the source and intensity of the stressor.
Due to a head injury or illness affecting the brain.
Psychosis triggered by the use of alcohol or illicit substances, such as stimulants (e.g., methamphetamine, cocaine), hallucinogenics (e.g., LSD), and synthetic cathinones (i.e., bath salts). Some prescription medications for treatment of pain or other mental health disorders can also cause temporary psychosis. Individuals with addiction may experience these symptoms if they suddenly stop drinking or using substances.
Individuals with this mental health disorder experience frequent and intense fluctuations in mood, varying between depression and mania. When their mood is manic, they may have symptoms of psychosis such as delusions of grandeur. When they are depressed, they may have symptoms that make them feel upset, frightened, or sad, such as delusions of persecution.
A mental health disorder in which the individual strongly believes in things that do not exist or are not true. The ongoing delusions they experience are not typically accompanied by hallucinations.
This involves Major Depressive Disorder (i.e., depression) that is accompanied by various psychotic symptoms. It occurs in approximately 20% of people with Major Depressive Disorder. In some cases, the content of their hallucinations and delusions are consistent with the depressive symptoms (e.g., feelings of guilt, self-criticalness). In other cases, their hallucinations and delusions do not pertain to their depression. Individuals with psychotic features are at increased risk of committing suicide. This disorder is similar to Bipolar Disorder, without the mania.
In rare instances, women may experience post-partum psychosis. The onset is within the first two weeks of the postpartum period and the course is typically brief. It is more likely to occur if the mother has a family history of a psychotic or mood disorder, or if she has had a prior psychotic episode. Most women with these symptoms do not harm themselves or anyone else, however, there is always risk of danger because the symptoms may include delusional thinking or irrational judgment.
A lifelong mental health disorder seen in approximately 1% of the population that involves the presence of multiple psychotic symptoms consistently for at least six months. It is also associated with impaired cognitive, social, and occupational functioning and changes in mood/thoughts.
Similar to Schizophrenia but also includes periods of depressive symptoms that occur only during the duration of the psychotic episode.
Similar to Schizophrenia in terms of symptoms, lasting at least a month but less than six months.
A personality disorder characterized by pervasive patterns of interpersonal difficulties. This typically includes discomfort with, and diminished capacity for, close relationships, as well as a lack of close friendships. It is also associated with delusions, hallucinations, paranoia, impaired thoughts/speech, odd behaviour, and restricted affect.
Myth: People with psychosis are unable to lead normal lives.
Fact: There are many people living with psychosis or a psychotic disorder who lead normal lives.
Many people with psychosis are able to live productive and meaningful lives. In fact, some individuals only have one or two short-term episodes and do not experience psychosis again. This is particularly if some of the psychosis triggers are able to be adequately addressed (e.g., stress, addiction, depression). Others are able to work with health professionals to develop successful long-term treatment strategies to help prevent future episodes and to cope with their symptoms should they develop. That is, the intensity and frequency of psychotic symptoms can be reduced with psychotherapy and medication to minimize the degree of functional impairment. In more mild cases, individuals may live independently with minimal external supports. In more severe cases, close monitoring/supervision and more intense intervention and support may be required (e.g., occupational therapist, recreational therapist, case worker, residential treatment program, etc.).
While it may not be possible to engage in activities of daily living during a psychotic episode, the frequency and severity of these episodes can be targeted with treatment. As a result, many individuals are able to be productive and participate in social/recreational activities between episodes.
Generally, the longer one has been living with untreated psychosis, the longer it will take for them to improve. As such, prevention strategies and early intervention are very important. Individuals who are most likely to benefit from early intervention include the following:
- Youth with positive psychotic symptoms.
- Individuals with transient psychotic symptoms that do not have a formal mental health disorder yet.
- Those with a genetic risk factor (i.e., family member with a psychotic disorder).
- Individuals with Schizotypal Personality Disorder showing signs of deterioration in functioning.
Treatment for psychosis typically includes a combination of medication and psychotherapy. Medications that are used to treat psychosis typically include selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, anti-psychotics, and/or benzodiazepines. These medications work by attempting to regulate neurotransmitters in the brain, thereby preventing future episodes of psychosis. For many individuals, they only need to take medication for a short period of time until their symptoms are diminished. However, if they have a psychotic disorder such as Schizophrenia, they may have to stay on medication for life.
Psychotherapy provides education to the individual and their family about psychosis. It also teaches the individual different strategies to cope and build their support network. There is a focus on long-term maintenance and stress management. Indeed, stress can heighten an individual’s symptoms and increase their impairment in functioning.
Cognitive behavioural therapy is an evidence-based treatment that focuses on the connection between our thoughts, behaviours, and emotions. It can be used to help an individual change the way they think about, and respond to, their hallucinations and delusions. The goals of therapy are to make the symptoms less distressing in the moment and less impairing on a daily basis (i.e., to improve quality of life).
Once treatment is initiated, positive psychotic symptoms are usually addressed and managed first. However, negative psychotic symptoms may linger over time, as they are less responsive to medication. Even with a good response to treatment, problems such as depression, addiction, decreased self-esteem, social/financial/housing problems, and difficulties with work/school may need to be concurrently addressed.
If your loved one has psychosis or a psychotic disorder, you are able to help. This individual may be scared, withdrawn, or uncertain how to handle their disconnect from reality. Support them non-judgmentally; listen and validate their concerns; and provide an understanding of the difficulties of their situation. Encourage them to seek help from mental health professionals. Provide them with feedback to outline how their symptoms are impairing their functioning if they lack insight; however, do not do this during a psychotic episode, as the individual may not comprehend you or be able to think rationally. Encourage strategies for general mental health, including stress management strategies (e.g., deep breathing, mindfulness, exercise), good personal hygiene, proper eating habits, avoidance of alcohol/illicit substances, etc.
Youth with Psychosis
While psychotic symptoms in children and adolescents are less common, youth with such symptoms can demonstrate impairment at school and with their family/friends. They may demonstrate a decrease in personal hygiene, withdraw from friends, feel suspicious of others, lose interest in activities, develop unusual ideas, have unusual perceptions, demonstrate a change in personality, or have difficulty organizing their thoughts or speech. Such individuals are more likely to have unmanaged stress, disrupted sleep, and prior mental health issues (e.g., addiction, anxiety).
With early assessment and intervention, most youth are able to manage their symptoms and address any triggers. As such, their symptoms usually fade over time or remain mild. A smaller portion of youth will go on to develop a psychotic disorder in the future. Overall, psychoeducation for the youth and their family, cognitive behavioural psychotherapy, medication, and stress management are key components in treatment.
Conclusion
In conclusion, psychosis can be caused by a number of factors, and present very differently depending on the individual. In some cases, psychotic symptoms are mild, transient, and easily managed; in others, symptoms are more severe and pervasive.
Did any of the dispelled myths pertaining to psychosis surprise you? Why or why not? Please comment below.